Nepal Training Program
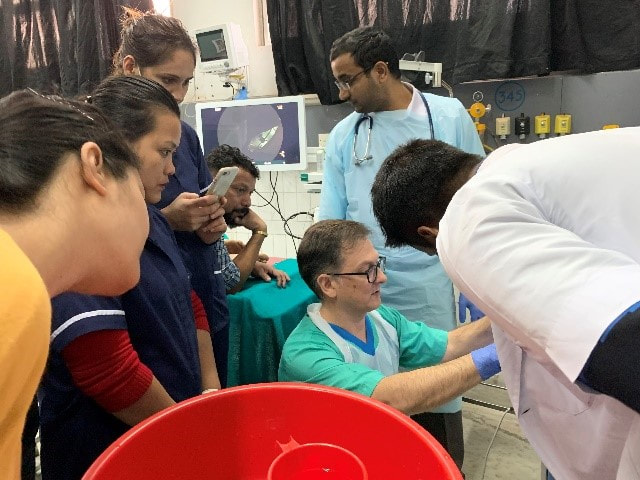
 Trainers and trainees, 2019 (photo John Masson)
Trainers and trainees, 2019 (photo John Masson)
ANZGITA NMC Program 2019: A Story of Building Sustainable Relationships
Report from ANZGITA Program Leader, Dr John Croese
The ANZGITA - NMC (Nepal Medical College) program completed its second year in Kathmandu in November 2019. This report on the visit includes consideration as to how we might build a sustainable program. An informal relationship between Australian and Nepalese gastroenterology has been developing since 2017 following visits by Ann Vandeleur, Dianne Jones, John Masson, Christine Welch, Tony Rahman and me. Fostering this relationship has been encouragement, advice and support from Prof. Sunil Kumar Sharma (NMC), Drs Satyam Rimal (NMC) and Punyaram Kharbuja (Bhaktapur Cancer Hospital), and many other senior Nepali clinicians and administrators.
In 2018, following an exploratory visit and negotiations conducted by Prof. Finlay Macrae and Assoc. Prof. Peter Katelaris, ANZGITA elected to formalise a training program located at NMC and the first week-long training program was held.
The 2019 team comprised previous visitors, Ann, Dianne, John Masson, Christine Welch and me, and Dr Mark Appleyard, a first timer. Our accommodation was very satisfactory with convenient transport provided by NMC, as well as the welcome option of a 40-minute walk to and from work.
Again, the training venue was the NMC, a general hospital established in 1997 through private capital to provide one of Nepal’s largest but most diverse undergraduate medical, nursing and allied health training programs. The endoscopic service at NMC had been the remit of general surgeons, but now includes a recently appointed young well-trained gastroenterologist, Dr Abashesh Bhandari, who is able to provide diagnostic and basic therapeutic endoscopy. His appointment had been too recent to have had an impact on patient load and service delivery at NMC.
Following discussions in 2018, a unit upgrade was completed during 2019 under the leadership of Dr. Satyam Rimal with the installation of a purpose-built endoscope reprocessing room and the refashioning of two adjoining clinical rooms. Reprocessing at NMC is manually based, but far superior to that available at most hospitals in Nepal and affords a unique opportunity for nurse training.
Nursing involvement this year was limited to NMC staff with subsequent attendance of a few personnel from units supported by senior clinicians previously involved with the program. A recurring shortcoming for safe reprocessing care has been the retention of dedicated staff and to this end a decision to retain trained nurses in endoscopy at NMC has been adopted in 2019 following ANZGITA's strong recommendation.
Medical attendance on the program was less than hoped with 4 to 6 novice and early trainees attending each day. (Up to 10 is ideal.) It was not clear why this occurred but it seemed some employers were concerned at the time needed on the program which led to the late withdrawl of some prospective trainees. For 2020 the training goals and training activities will be planned in more detail and more clearly communicated. Closer co-ordination with other hospitals and services will provide a higher caseload for the anticipated number of trainees. Dr Bhandari's recruitment and the support of senior NMC personnel will assist with this.
The attending medical and surgical trainees received very personalised training. They all remained completely engaged and found the week a productive and possibly even a life-changing event. They proved a delight to train and interact with. Equally, the ANZGITA team was superb. The course concentrated on supervised reprocessing, hands-on clinical and mannequin skills training, and interactive discussions based on the day’s clinical events and technical aspects of safe endoscopy. The quality of training provided was both a reflection of the trainers’ skills and their deep commitment to education.
Drs Masson and Welch with DM trainee Dr Karki Dr Appleyard teaching safe diathermy
The team was extravagantly entertained by the trainees. We visited the family home of one for dinner and another devoted a free day to escorting us at his expense sightseeing. Prof. Sharma hosted the team to a private dinner, which was delightful and extremely productive providing insights into the dynamics of healthcare in Nepal. Dr Satyam Rimal and the NMC Board of Directors hosted a formal evening with trainees and trainers to close the program and recognise the attendance of the trainees. Prof. Sharma and the NMC Board are committed to the program and the success of the 2020 program.
There is no quick remedy for gastroenterology in Nepal. Economic constraints dictate that most endoscopy is performed by doctors with limited training, on patients without sedation and with poor equipment that has not been adequately cleaned between cases. Substantive change will take many years and will require consistent international support. The 2020 visit will be the third program and consist of 3 doctors and 3 nurses working with up to 10 physician trainees and a similar number of nurses. This seems a very modest response to an overwhelming situation, but it is consistent with ANZGITA’s capacity to deliver and it is a proven model. With reinvigorated support from the NMC Board and its clinicians, the ANZGITA program can work by investing in the next generation of locally trained Nepali nurses and doctors the awareness of how endoscopy should be performed, and the skills necessary to practice and teach safe endoscopy.
To help ensure 2020 is a success, funding is now required to maintain the program, and regular engagement between ANZGITA and NMC is necessary to develop an agenda, to promote the week targeting hospitals with gastroenterology services and to ensure timelines are met. This needs to occur at a nursing and a medical level. Program Leaders from both NMC and ANZGITA will work closely on achieving these goals.
The program needs to be clearly defined. I would suggest 3 themes: reprocessing (10 nurses), endoscopy for novices (6 doctors) and polypectomy/endoscopic mucosal resection for intermediate operators (4 surgeon/GE physician trainees). This very specific focus on polypectomy will help define case selection, address colon cancer which is an emerging problem in Nepal and improve local expertise. Observation from previous visits suggests polypectomy even in more experienced hands is very poorly managed. Early engagement with the directors of gastroenterology at other hospitals emphasising a week’s intensive hands-on training in the latest technique in endoscopic polypectomy will be an attractive proposition to them.
The team was extravagantly entertained by the trainees. We visited the family home of one for dinner and another devoted a free day to escorting us at his expense sightseeing. Prof. Sharma hosted the team to a private dinner, which was delightful and extremely productive providing insights into the dynamics of healthcare in Nepal. Dr Satyam Rimal and the NMC Board of Directors hosted a formal evening with trainees and trainers to close the program and recognise the attendance of the trainees. Prof. Sharma and the NMC Board are committed to the program and the success of the 2020 program.
There is no quick remedy for gastroenterology in Nepal. Economic constraints dictate that most endoscopy is performed by doctors with limited training, on patients without sedation and with poor equipment that has not been adequately cleaned between cases. Substantive change will take many years and will require consistent international support. The 2020 visit will be the third program and consist of 3 doctors and 3 nurses working with up to 10 physician trainees and a similar number of nurses. This seems a very modest response to an overwhelming situation, but it is consistent with ANZGITA’s capacity to deliver and it is a proven model. With reinvigorated support from the NMC Board and its clinicians, the ANZGITA program can work by investing in the next generation of locally trained Nepali nurses and doctors the awareness of how endoscopy should be performed, and the skills necessary to practice and teach safe endoscopy.
To help ensure 2020 is a success, funding is now required to maintain the program, and regular engagement between ANZGITA and NMC is necessary to develop an agenda, to promote the week targeting hospitals with gastroenterology services and to ensure timelines are met. This needs to occur at a nursing and a medical level. Program Leaders from both NMC and ANZGITA will work closely on achieving these goals.
The program needs to be clearly defined. I would suggest 3 themes: reprocessing (10 nurses), endoscopy for novices (6 doctors) and polypectomy/endoscopic mucosal resection for intermediate operators (4 surgeon/GE physician trainees). This very specific focus on polypectomy will help define case selection, address colon cancer which is an emerging problem in Nepal and improve local expertise. Observation from previous visits suggests polypectomy even in more experienced hands is very poorly managed. Early engagement with the directors of gastroenterology at other hospitals emphasising a week’s intensive hands-on training in the latest technique in endoscopic polypectomy will be an attractive proposition to them.
Nepal Backgound
 Bearing and receiving gifts - Ann Vandeleur and Di Jones at NMC on their fourth visit in four years, an incredible commitment. The pomelos were a gift from one of this year’s trainees
Bearing and receiving gifts - Ann Vandeleur and Di Jones at NMC on their fourth visit in four years, an incredible commitment. The pomelos were a gift from one of this year’s trainees
Nepal is a small nation located in the Himalayas, landlocked by China (predominantly Tibet) to the north and India to its south. The population is estimated to approach 30 million. It is ethnically and spiritually diverse, and whilst agriculture provides half the national employment, the majority live in a sprawling and hectic Kathmandu (KTM), the national capital. It is one of the poorest nations in the world with around 40 percent living in poverty. Serious damage resulted from the earthquakes in 2015 which killed more than 7,000 people and injured another 14,000. Huge damage was caused to the infrastructure in the capital and the countryside, and the economy suffered. Remarkably, the resilient Nepalis remain tolerant and get on with the business of living.
Disease burdens in Nepal are poorly defined due to a lack of data, the country suffering the lowest expenditure on medical research of all subcontinent nations, about 0.01% of an already meagre GDP. It does appear though that, as in developed nations, disease patterns are changing with reductions occurring in communicable, neonatal and nutritional disease rates whilst non-communicable disease and injury rates are static. Liver disease associated with hepatitis C, illicit drug use and alcoholism, gastric cancer and cervical cancer rates remain very high. Anecdotal evidence of an increase in colorectal cancer rates in young people is emerging.
Medical and nursing education, although loosely structured around numerous government supported and private colleges, is good, consistently producing young doctors and nurses who are readily employed overseas, many of whom migrate never to return. Specialist medical education generally occurs overseas, in western facilities, and more recently in India and China, where the attraction to remain must be difficult to resist. For these excellently trained Nepali physicians and surgeons, many must ply their trade in climate of inexhaustible demand, and often in poor facilities with limited equipment. Most hospitals struggle to provide reliable water and electricity, let alone well equipped and maintained endoscopy units. Endoscopy services are very limited, and consequently there is an unmet demand to train competent endoscopists.
ANZGITA's involvement follows on from the work started by Dr John Croese and doctor and nurse colleagues soon after the 2015 earthquake. John and a small team including two experienced ANZGITA nurses, one being our nursing director Dianne Jones, returned in 2017. John championed the involvement of ANZGITA and the establishment of a regular program of training. Following a visit by Finlay Macrae, Chair, and Peter Katelaris, Curriculum Director, the Board endorsed a small initial program for November 2018 in partnership with the Nepal Medical College (NMC) where Assoc Prof Satyam Rimal is the director of the endoscopy unit and a senior administrator. John Croese accepted the role of Program Leader with the support of Tony Clarke, Deputy Chair and programs co-ordinator. The NMC is a teaching hospital affiliated to Kathmandu University and wishes to develop a post-graduate DM course in gastroenterology with the support of ANZGITA.
Disease burdens in Nepal are poorly defined due to a lack of data, the country suffering the lowest expenditure on medical research of all subcontinent nations, about 0.01% of an already meagre GDP. It does appear though that, as in developed nations, disease patterns are changing with reductions occurring in communicable, neonatal and nutritional disease rates whilst non-communicable disease and injury rates are static. Liver disease associated with hepatitis C, illicit drug use and alcoholism, gastric cancer and cervical cancer rates remain very high. Anecdotal evidence of an increase in colorectal cancer rates in young people is emerging.
Medical and nursing education, although loosely structured around numerous government supported and private colleges, is good, consistently producing young doctors and nurses who are readily employed overseas, many of whom migrate never to return. Specialist medical education generally occurs overseas, in western facilities, and more recently in India and China, where the attraction to remain must be difficult to resist. For these excellently trained Nepali physicians and surgeons, many must ply their trade in climate of inexhaustible demand, and often in poor facilities with limited equipment. Most hospitals struggle to provide reliable water and electricity, let alone well equipped and maintained endoscopy units. Endoscopy services are very limited, and consequently there is an unmet demand to train competent endoscopists.
ANZGITA's involvement follows on from the work started by Dr John Croese and doctor and nurse colleagues soon after the 2015 earthquake. John and a small team including two experienced ANZGITA nurses, one being our nursing director Dianne Jones, returned in 2017. John championed the involvement of ANZGITA and the establishment of a regular program of training. Following a visit by Finlay Macrae, Chair, and Peter Katelaris, Curriculum Director, the Board endorsed a small initial program for November 2018 in partnership with the Nepal Medical College (NMC) where Assoc Prof Satyam Rimal is the director of the endoscopy unit and a senior administrator. John Croese accepted the role of Program Leader with the support of Tony Clarke, Deputy Chair and programs co-ordinator. The NMC is a teaching hospital affiliated to Kathmandu University and wishes to develop a post-graduate DM course in gastroenterology with the support of ANZGITA.
|
| ||||||||||||